[google-translator]
Today’s post is co-authored by Jess Steele, Director of Outcomes and Evaluation, and Dan Lakin, Outcomes and Evaluation Clinical Manager, at Uplift Family Services. Their roles are to support data collection, entry, and reporting agency-wide, in addition to working closely with staff to interpret and learn from their program outcomes in order to enhance the quality of service delivery for children and families.

Within a week of California’s shelter-in-place mandate, Uplift Family Services pivoted to an agency-wide implementation of telehealth—conducting behavioral health services using phones or video conferencing software, with our staff largely working from home.
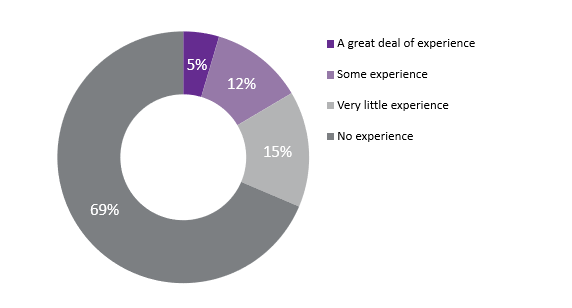
This transformation was essential to ensure we could continue providing customers with timely, high quality, and essential services during a time of profound psychological distress for many of the youth and families we serve. It also represented a giant leap into the unknown for the agency—telehealth was not only new to over 80% of our clinical staff but is also largely under-researched. There were very few experts to turn to for guidance around best practices for customer engagement while delivering services remotely.
Telehealth Transition by the Numbers
This May, we sent surveys to the families of our children and teens, as well as our staff who are providing care via telehealth, to better understand how each group was navigating COVID-19 and the switch to telehealth as our primary means of therapeutic communication. We received 349 responses from families and 332 from staff.
We collected information related to individual experiences with telehealth, needs for additional training and support, as well as well-being, burnout, and shifts in management strategies for our staff. Some highlights from the survey include:
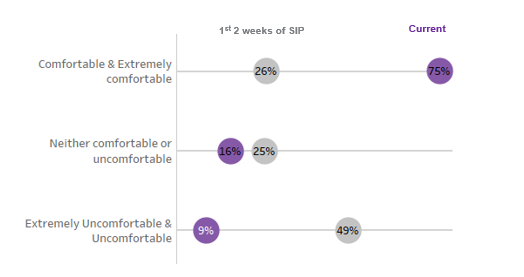
- Staff levels of comfort with telehealth increased from 26% to 75% within a few weeks, underscoring their adaptability and creativity, in addition to the robust resources and trainings we quickly rolled out agency wide
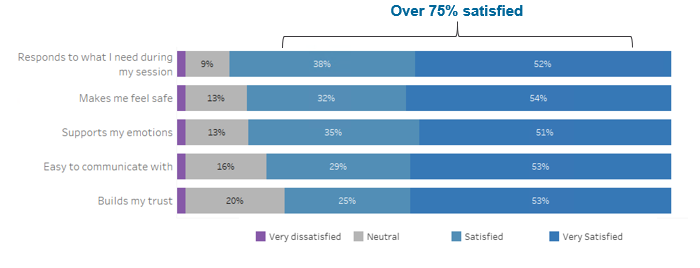
- Over 75% of youth and families reported they were thus far satisfied with both their overall experience with telehealth and their provider’s ability to deliver sessions remotely
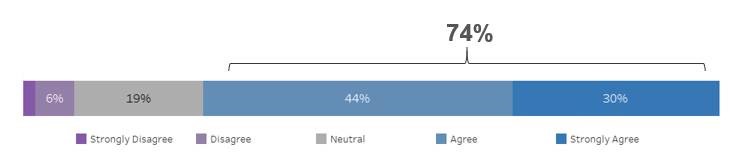
- 74% of customers shared they felt they were making just as much progress toward treatment goals using telehealth as they were during their in-person sessions
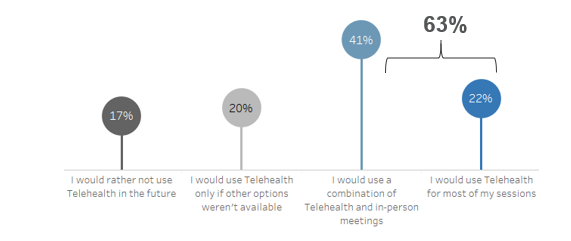
- Over 60% of staff and customers would opt in to using telehealth in the future, even if in-person services are an option
A parent of one of our youth summarized their experience with telehealth by saying:
“I think telehealth has dramatically improved our services because we are able to schedule more easily and we are able to decompress quickly after intense or emotionally demanding sessions by just sitting on the sofa or cooking together. While I think in-person occasionally would be useful, telehealth has shown me that my daughter can still heal and grow with her therapist and behaviorist even if it’s by phone. It’s actually made her more comfortable in sessions because she’s in a familiar environment.” —Caregiver in Los Angeles
The Impact of Telehealth on our Staff and Community
It has been exciting to see the enormous efforts of our entire agency pay off, and to learn that customers and families were largely satisfied with their experience with remote service delivery. Not surprisingly, however, there were also costs associated with the pandemic and resulting rapid transition to telehealth.
Our agency saw a 16% average reduction in our ‘units’ of service delivery—the number of sessions received multiplied by the time spent in session—during the shelter-in-place order, through the end of June 2020. While the frequency of appointments each week increased, the average length of each appointment decreased, suggesting that therapists were making more attempts to contact their clients but having a harder time keeping them engaged for long periods of time in remote sessions.
The lack of evidence-based best practice guidelines for telehealth sessions also took a toll on staff. A large majority of respondents expressed a need for training in specific intervention modalities that work well within a telehealth framework, and strategies to more readily engage families in therapy—how to get them to pick up their phone/sign into a telehealth platform, or how to keep them in their chair once they’ve agreed to talk.
Where Do We Go from Here?
Telehealth will likely become a more permanent part of the behavioral health delivery landscape. As an agency, the importance of improving our ability to deliver high-quality remote services and contribute lessons learned to the behavioral health community is increasingly evident.
We recently started a “Phase II” interagency telehealth workgroup to build upon our learnings from March to July and develop a set of concrete metrics. These metrics will be used to measure our progress and understand the impact of telehealth on outcomes for our youth and families.
We are also collaborating with other agencies to understand their own implementation challenges and successes, and advocating at the local, state, and federal level to ensure we are building reimbursement models that ensure the sustainability of mental and behavioral care delivery far into the future.
We are excited to see what the future of telehealth holds!